The Secret To Polio Eradication In India
This post was originally produced for Forbes.
On March 26, 2014, the World Health Organization (WHO) is expected to certify India as a polio free country, marking more than three years since the last case of polio there. While visiting India for this story as a guest of Rotary International, I stumbled upon a surprising secret—more about that later.
It is virtually impossible to convey the magnitude of the eradication of polio from India. Deepak Kapur, a business leader in New Delhi who has chaired Rotary’s National PolioPlus Committee in India since 2001, explained the challenges to me during my recent visit. He identified six major challenges that the country faced:
Population: The biggest challenge is the sheer scale of the project, needing to vaccinate 172 million children twice each year. Note that there are only seven countries with a total population greater than 172 million on the planet.
Population Density: On one immunization visit, Kapur noted 107 people living within a 30 square yard plot of land in shanties, literally taking sleeping shifts around the clock.
Insanitary Conditions: You can see refuse flowing in open sewers and otherwise abysmal sanitation conditions in many Indian communities, especially in Utter Pradesh and Bihar.
Impure Drinking Water: Many people in India still lack access to clean drinking water; they may be drawing water from shallow wells in places with no sewer system such that there is a constant intermingling of sewage and drinking water.
Malnourishment: Malnourished children don’t seem to get the same immunity from the vaccine that healthy children get. In the developed world, children receive three doses of the vaccine and gain immunity. Some Indian children have been infected with the virus after 18 documented doses.
Enteric diseases: Several communities in India have the highest incidence of enteric diseases in the world, meaning that the kids who received an oral dose of vaccine wouldn’t gain immunity due to diarrhea—the vaccine simply didn’t stay in the body long enough to do any good.

Deepak Kapur, a business leader in New Delhi
Without seeing, smelling and hearing these problems in person it is difficult to get a complete sense of the challenges. Having been there, I can tell you that only having it done makes it seem possible.
(The story continues after the infographic.)

Courtesy of InfoGraphicWorld.com
The Secret:
Sajjan Goenka, an entrepreneur and philanthropist in Mumbai who has been a member of Rotary since 1968 was the first person I interviewed in India for this story; he shared the surprising secret with me. He shocked me when he said, “We didn’t believe we could do it. I didn’t believe we could do it.” Kapur agreed, offering up the same observation after he enumerated all of the challenges to eradicating polio.
I expected bravado and chest thumping. I expected to hear that “we always knew we could do it.” In fact, a group of naïve, well-intentioned people got together and thought even though it would probably be impossible, it was important enough to try.
And so it—the eradication of polio from India—is done. In the 1980s, there were approximately 350,000 cases of polio every year worldwide, 150,000 in India. In 2013 there were just 403 cases of polio worldwide, none in India, according to a WHO report.
Goenka was the first to help me understand the early history of the fight against polio. In those early days in the 1980s, he explained, Rotary was virtually alone in the effort. He explained that the government was not investing in polio vaccines so Rotary funded and administered the first vaccination campaigns alone.

Sajjan Goenka, Rotary member, entrepreneur, philanthropist
Over the years, the Centers for Disease Control (CDC), the WHO, UNICEF and the Indian Government all got involved. More recently, the Bill and Melinda Gates Foundation (BMGF) has added more than $1.5 billion to the fight in an effort to ensure that having come so far, the virus is finally defeated.
The Vaccine:
Dr. Sunil Bahl, Deputy Project Manager, National Polio Surveillance Project (NPSP), a joint project between the Indian Government and WHO, explained some of the technical challenges of the polio vaccine. There are—or were—three strains of Polio, commonly called P1, P2 and P3. For more than a generation, a “trivalent” vaccine that inoculated against all three strains was used.

Dr. Sunil Bahl, Deputy Project Manager, National Polio Surveillance Project
In India, however, it was learned through the NPSP surveillance that the trivalent vaccine was not especially effective. Children weren’t gaining immunity. The last case in the world of P2 was reported in 1999, so thereafter it was no longer necessary to immunize against it. So, in 2005, the country began using “monovalent” vaccines that inoculated against just one strain. The results were immediately apparent. When the P1 vaccine was used, cases of P1 dropped significantly, but cases of P3 would rise.
A “bivalent” vaccine had not been developed or used prior to that point. The bivalent vaccine was developed in 2009 and it is now used around the world. Its efficacy is comparable to the monovalent vaccines—much better than the trivalent vaccine—and it covers the last two strains.
Dr. Jay Wenger, a Director of Global Development at the BMFG who previously worked with Dr. Bahl, explained that the last reported case of P3 occurred just over one year ago. Only P1 appears to be surviving today.
Government of India:
Everyone I spoke with was quick to give the ultimate credit for success in India to the Indian Government. When I met with Anaradha Gupta, An Additional Secretary in the Ministry of Health and Family Welfare who serves as the Mission Director of the National Rural Health Mission (NRHM), leading the polio fight for the Indian Government, I was impressed that I had found the person responsible for finally snuffing the life out of polio in India.

Anaradha Gupta, An Additional Secretary in the Ministry of Health and Family Welfare
Gupta earned an MBA in Australia and has done executive education at both Stanford and Harvard. It showed. She spoke the language of an MBA, focused on process and outcomes. When she took office in 2009, India had 741 cases of polio. In 2010, there were just 42 cases, with the last case of polio in India reported in January 2011.
She explained that early in her tenure, she faced a difficult decision. The World Bank was prepared to provide funding for vaccines in 2010. The loan would come with strings attached. One of the strings was that vaccines were to be purchased from WHO prequalified manufacturers, who were not yet prepared to produce the vaccine at the scale required for India. Gupta decided to source the vaccine locally in India from high-quality, but non-WHO-prequalified who met India’s “Good Manufacturing Practices.” The impact of that decision is evident in the dramatic decline in cases from 2009 to 2010 and 2011. “We saw amazing results,” she exclaimed.
The other key, she says, was the programmatic effort to ensure that every single child was immunized. The goal was to reach every single child. Her data indicates that they in fact reached 99.7 percent of the children under five in the country. “We started to get data of every household that was missed,” she explained.
National Immunization Days:
The government organizes, with help from Rotary, WHO, and UNICEF, two National Immunization Days (NIDs) each year. On these days, all 172 million children are immunized. Volunteers from Rotary work side-by-side with health care workers to stand up immunization booths in every community in the country. In the days leading up to the event, all sorts of promotion is done.
Scott Leckman, a cancer surgeon from the Salt Lake Rotary Club (my club) has been visiting India every year for the past five years to help with the NIDs. He noted that on the day before the NID, he works with local Rotary clubs to distribute flyers around the community to alert people to the place and time for the NID booth in the community the following day.
When I visited India, I was able to observe a rally with about 100 Rotarians, many local, plus groups from Tokyo Japan and Devon, England, along with 300 primary and secondary school students. The group, with visiting Rotarians riding horses, a marching band playing, marched through the neighborhood for two hours waving signs and banners announcing the NID place and time.

Immunization Day Rally through poor neighborhood in Delhi, India
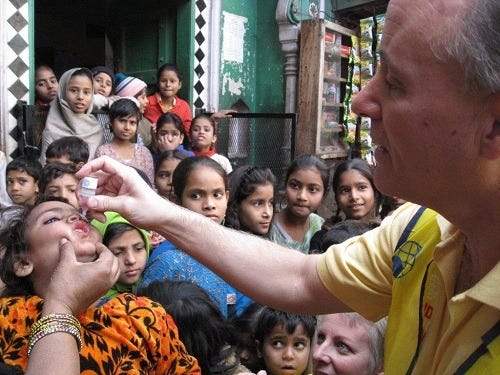
On the actual day of the event, I visited three booths operating in strategically different ways. The first stationary booth was, as it was explained, the most common sort. Set up under a simple awning, Rotary volunteers working with health workers began immunizing children with two drops of the oral vaccine early in the morning. Each child immunized would receive a toy ball. Given the incentive, it was not surprising to see that most of the young people were accompanied by modestly older siblings; six-year-olds dragged their four-year-old brothers and sisters to get inoculated in order to get the toy ball.

Dr. Mona Khanna immunizes children in Delhi, India
When children were immunized, their pinkies were marked with a pen using the same ink used to mark adult fingers after voting in an election here in India. This not only prevents children from being immunized multiple times for the sake of toys, but also allows for the “mop-up” teams who go house-to-house following the NID to find the children who weren’t immunized.
On the NID, there are also mobile units that drive around setting up shop quickly and then moving on after immunizing the children in the immediate area.
The third focus of the NID is transit stations; booths are set up in train stations. The workers and volunteers there not only invite children passing through the stations be immunized, but also board the trains when they stop in the station to look for children who need to be immunized and give them their drops right on the train.
Leckman shared with me an anecdote from his 2009 trip with 16 Salt Lake Rotarians to India to help with the NID.
Dr. Scott Leckman, Rotary Member, immunizing children in India
After doing the immunizations and walking back to the bus. I’m kind of walking by myself and this Indian guy about my age on a bike was passing by and jumps off and starts walking with me.
He says, “Where are you from?”
I say, “The United States.”
“What are you doing here?”
“I’m with Rotary and we’re immunizing kids against polio.”
“Well, what do you get out of it?”
I said, “A world without polio.”
He thought about it for a moment and simply replied, “Namaste,” which is to say, I recognize the divinity within you. Then he got back on his bike and rode away.
Polio’s Impact:
Since Rotary launched its effort to eradicate polio in 1985, approximately 10 million cases of polio have been prevented. For many in the developed world, however, that is a statistic without much meaning. Few people younger than 50 even know of anyone personally who was afflicted with polio-related paralysis.
During my visit to Delhi, I visited St. Stephen’s Hospital, which operates the only dedicated polio ward in India. The program is led by Dr. Mathew Varghese, who gave us a tour of the ward.

Dr. Matthew Varghese with one of his patients in the cancer ward
Polio frequently paralyzes the lower limbs and most often impacts those with little economic means, leaving them in the humiliating position of being forced to crawl. The kids who grow up crawling end up with permanent deformities.
Dr. Varghese accepts every patient who comes to him, regardless of ability to pay. Over the last decade, he boasts enthusiastically, that his patients are getting older and older. Virtually all of his patients are now over 15. He performs surgeries that allow children who crawl, to stand and walk in braces or calipers. Some children have had paralysis on only one leg. One outcome is that the affected leg is shorter than the other leg. Dr. Varghese provides surgery to lengthen the leg one millimeter per day. This allows patients to get out of orthopedic shoes and sometimes to eliminate the need for crutches or even a cane.
The ward is financially supported by Rotary.
The History of Rotary’s Fight to End Polio:
One of the highlights of my visit to India, was a meeting with Raja Saboo, who at the age of 80 interrupted his planning for a humanitarian mission to Rwanda, to visit with me.

Raja Saboo, former President of Rotary International
Saboo served as the President of Rotary International in 1991-92; he joined Rotary in 1961. As a young man, he met Mahatma Gandhi and as an adult met Mother Teresa several times. In 1992, he visited South Africa in his official capacity as the President of Rotary International. He was surprised to be invited to meet with President F. W. de Klerk. After a brief introduction, the South African President invited Saboo to stand with him at a press conference where he announced the end to apartheid.
Saboo, who served on the Rotary International Board beginning before the decision to make polio Rotary’s global effort, was able to provide a historical perspective.
Individual Rotary clubs were engaging in the fight against polio by the late 1970s, but this work was all being done at the club level and not at the international level.
Sir Clem Renouf of Australia served as the president of Rotary in 1978 and 1979 was the first to identify polio as a potential large scale project for Rotary. In 1981, Rotary decided approve a proposal to “immunize the children of the world against polio by 2005, when Rotary would be celebrating its 100 years. In 1988, the goal was rephrased as the eradication of polio, a difference that may be viewed as symbolic, but was actually a significant leap. No longer would success be judged by Rotary’s effort, but by the outcome.
When Rotary first estimated the cost of the program, Saboo said, the organization estimated the cost would be $25 million. They quickly realized that the cost would be much higher, estimating that it would be at least $120 million. In 1988, Rotary International raised $240 million to kick off the effort in earnest.
More than $10 billion has been spent to date to end polio with a budget of approximately $5 billion pending for the “Endgame Strategic Plan.”
Saboo played a key role in managing one of the biggest challenges of the immunization campaign. Some people in the Muslim community were especially resistant to efforts to immunize their children. Saboo visited a community where five families were specifically identified who were refusing to have their children vaccinated. During the visit, Saboo noticed a small child crawling on the ground in a classic polio afflicted way. He recognized that the child needed polio corrective surgery. He organized an effort to have this child and other children in the area receive the needed surgeries. This helped to soften the resistance to immunizations.
Public Relations:
In India, managing the challenge of public relations is the primary responsibility of UNICEF. During my visit, I sat down with Nicole Deutsch, Chief of Polio with the UNICEF India Country Office.

Michelle Kloempken, Rotary, Nicole Deutsch, UNICEF, Nima Chodon, Rotary
“UNICEF’s role is primarily on the social mobilization and communications side; this is about creating demand for the vaccination and raising awareness about its benefits,” Deutsch explained. Deutsch noted that she previously worked in Nigeria on polio and that while there, they used the “India Model” of communication for building community support.
Much of the focus is on bringing in influential leaders, like religious and local political leaders and doctors to participate in local functions to establish credibility for the immunizations.
“Branding was a big thing in India; so anytime people saw the pink and yellow they knew a campaign was being announced,” she explained. She highlighted the use of celebrities as spokespeople for the campaign across all sorts of media, including text messages.
“At one point it became obvious that there were certain communities that were being repeatedly missed or had distrust. Working with Islamic leaders and imams really helped turn things around. They were a major force in getting community buy in and support for this. Rotary had actually done a council of Ulemas to meet one time,” she noted.
Deutsch made it clear that the success in India came down to creating a universal understanding and agreement important among local and national government and among religious leaders that immunizations were. Everyone took ownership of the program within their particular responsibility.
The Legacy of the Polio Campaign:
With the eradication of polio in India and the imminent end of polio globally, it may be too early to look at what’s next, but it is clear that the 30 year effort to end polio has proven a few things. Most importantly, we can see that there is a way for humankind to do extraordinary things. In many ways, ending polio has proven to be a much greater challenge than going to the moon and yet we can predict reasonably that the final case of polio in human history will be reported in the next twelve to 18 months.
Dr. Wenger from the BMGF explained the Foundation’s hope that the “personnel and machinery used for the eradication of polio will be used for other things,” like routine immunizations for DTP and measles.
“In India especially—when I was there in early 2002, the routine immunization coverage in Bihar was about 10 percent, so only 10 or 11 percent of kids were getting the vaccines they were supposed to get. After years of working on that not just with the polio folks—with other groups too—now 70 or 80 percent of children are getting vaccinated,” Dr. Wenger explained.
“We think that is a huge piece of the polio legacy to see that the infrastructure is used to help other health goals. That is a huge benefit of eradication,” Dr. Wenger said.
“The challenges in India were so stunning. You could really go to places in India and find thousands of kids living on top of each other without any sanitation and who were getting no health care. We would run into some areas where the only thing people were getting from outside was the polio vaccine. In a way, this is sort of sad. In some ways, it was evidence of the reach of the polio program.”
He noted that the NIDs required two million volunteers. “That’s a huge commitment and buy in by the population. Once you’ve done that for something, you should be able to extend that to other things. That would be the real benefit of polio eradication, even bigger than the bottom line thing of getting rid of polio,” Dr. Wenger concluded.
The post The Secret To Polio Eradication In India appeared first on Your Mark On The World.


